-
Preserving Your Eyesight as You Age
September is Healthy Aging Month, and people of all ages and walks of life are invited to participate. After all, good health in your golden years starts with a commitment to preventive wellness earlier in life. And if you’re already eligible for an AARP card, it’s never too late to get serious about your wellness. As you celebrate each passing year, you should pay attention to the changing needs of your eye health. In Chicago, eye doctors encourage patients to schedule regular exams, even if they don’t wear eyeglasses or contact lenses.

Schedule an eye exam.
Your ophthalmologist will let you know how often you should schedule an eye exam. If you’re 65 or older, you’ll probably need one every year or two. A comprehensive eye exam is an opportunity for the doctor to check for potential red flags of eye disease. With early treatment, it’s possible to delay the progression of eye diseases. It isn’t always easy to remember to schedule an appointment that only happens every year or two. Solve this problem by making your next appointment before you leave the optician’s office, and check that the office will send you a reminder card or email.
Wear sunglasses.
Sunglasses are much more than just a fashion statement. They can protect your eyes from the harmful ultraviolet (UV) rays. UV light increases the risk of cancer, cataracts, and growths on the eye. Look for sunglasses that offer broad-spectrum UV protection, and wear them each time you go outdoors. If you wear prescription eyeglasses, you can visit an optical center to order prescription sunglasses. Wearing a wide-brimmed hat can also help shield your eyes.
Quit smoking and avoid secondhand smoke.
There are dozens upon dozens of compelling reasons to quit smoking, including its detrimental effects on eye health. Smokers are more likely to be diagnosed with macular degeneration, cataracts, and dry eyes. They’re also at a higher risk of cardiovascular diseases, which can indirectly worsen eye health. It’s never too late in life to quit smoking. Consider it an investment in your future, just like saving for retirement. If you don’t smoke, don’t start. Avoid being near anyone who is smoking, as secondhand smoking is also harmful.
-
Exploring Your Glaucoma Treatment Options
An optic nerve transmits impulses from each eye to the brain. This allows the information that enters the retinas to be interpreted by the brain. The optic nerve is essential for your clear, healthy vision , and if this nerve sustains damage, blindness can result. Glaucoma refers to a group of eye problems that involve damage to this crucial nerve. If you’ve been visiting an ophthalmologist in Chicago for regular eye exams, then you’re more likely to be diagnosed with glaucoma early on. Your eye doctor can get you started on treatments to delay the progression of vision loss.

Medicated Eye Drops
Most people diagnosed with glaucoma start their treatment with prescription eye drops. There are different classes of medicines that can treat glaucoma, including the following:
- Beta blockers
- Prostaglandins
- Alpha-adrenergic agonists
- Carbonic anhydrase inhibitors
- Miotic or cholinergic agents
These eye drops regulate the pressure within your eye, which is called the intraocular pressure. By preventing the intraocular pressure from rising too high, the eye drops can delay or halt further damage to the optic nerve.
Oral Medications
Sometimes, eye drops by themselves aren’t sufficient to get the intraocular pressure down to ideal levels. The ophthalmologist might prescribe an oral medication to take in addition to your eye drops. Before taking any new medication, make sure your eye doctor has current information regarding your other prescriptions and medical conditions.
Laser Treatment
Another treatment option for glaucoma is laser surgery. If you have open-angle glaucoma, your doctor may perform a trabeculoplasty. He or she will use a special laser to improve the drainage of the intraocular fluid to reduce the pressure. Another laser surgery is an iridotomy, which is appropriate for patients with angle-closure glaucoma. This treatment also improves the drainage of intraocular fluid.
Eye Surgery
An ophthalmologist may recommend surgery performed without the use of lasers. One option is the implantation of a very tiny drainage tube. The surgeon will also create a reservoir underneath a thin membrane called the conjunctiva. The tiny tube sends intraocular fluid to the reservoir, and from there, the fluid absorbs harmlessly into the blood vessels.
-
How Is Glaucoma Diagnosed?
Visiting your local optical center in Chicago for routine checkups with an eye doctor is important for protecting your vision and practicing good eye care. However, this is particularly true for individuals over age 40. At this stage in your life, you have a greater risk of developing glaucoma.
Glaucoma is an eye disease that causes damage to the optic nerve. Because many people do not experience any glaucoma symptoms until the damage is significant, it’s important to schedule routine checkups with an ophthalmologist. To diagnose this condition, he will perform a comprehensive eye exam to check your peripheral vision, measure your eye pressure, measure your cornea’s thickness, examine your eye’s drainage angle, and measure or image your optic nerve.
If your optic nerve has already suffered damage due to glaucoma, then this cannot be reversed. However, your ophthalmologist may recommend laser surgery, medication, or glaucoma surgery to help slow the progression of the disease and preserve your remaining eyesight.

-
Glaucoma: How to Protect Your Vision
Glaucoma develops when the optic nerve sustains damage. Usually, glaucoma is the result of excessively high levels of intraocular pressure, or eye pressure. It develops slowly, which is why most people diagnosed with glaucoma are older adults. Although glaucoma is a major culprit of blindness in the U.S., there isn’t a cut-and-dry way to prevent it. However, you can talk to an ophthalmologist located in the Chicago area about your risk factors. By knowing your risk factors, your ophthalmologist can help you learn ways of protecting your eyes.
Visit Your Eye Doctor Regularly for Exams
When glaucoma is allowed to progress untreated, the vision loss is irreversible. Visit an optical center regularly to get your eyes checked. Your eye doctor will let you know how often you should schedule an exam, based on your individual risk factors. In general, glaucoma tests are recommended every 2 to 4 years before age 40. After age 40, you should be tested for glaucoma more frequently. Early detection of this vision problem allows for early treatment, which can slow the progression of vision loss.
Wear Protective Eyewear
Some people develop glaucoma not because of high intraocular pressure, but because of severe eye injuries that damage the optic nerve. These include injuries from caustic chemicals and flying projectiles. Ophthalmologists strongly recommend wearing protective eyewear whenever you’re doing a high-risk activity. These include using power equipment like chainsaws, mowing the lawn, doing carpentry work, and playing sports. Eye injuries can also occur from activities that aren’t generally seen as dangerous, such as using chemical cleaners in the kitchen.
Lead an Active Lifestyle
It’s thought that exercising regularly may help lower the pressure in the eyes . Researchers do not think that exercise has a lasting protective effect. In other words, exercise may only help if you continue to do it throughout your lifetime. Experts recommend moderate exercise at least 3 times per week. If you do yoga, try to avoid poses that invert your body. Headstands may increase your intraocular pressure.
-
Spotlight on Helen Keller Deaf-Blind Awareness Week 2017
There are people in the world who face extreme obstacles daily, and many of us can’t even imagine the struggles they go through. Helen Keller is an excellent example of someone who combatted serious handicaps in both deafness and blindness, and there is much to learn from her story. While a cataract surgeon or eye doctor in Chicago will have intimate knowledge of blindness, most people have a great deal to learn. Keep reading as we put the spotlight on Helen Keller Deaf-Blind Awareness Week 2017.
No matter how well our intentions may be, we can only focus our efforts on solving a problem after we’ve become aware of it. Most people over a certain age understand what deafness and blindness are, but there is much more to learn about these conditions. When you go about your daily life, you might not think about what your normal routine would be like without one or more of your senses. The purpose of Helen Keller Deaf-Blind Awareness Week is to take a week out of each year to discuss the presence of deaf-blindness in families within our communities so we can all widen our perspectives.

-
Get the Facts About Glaucoma
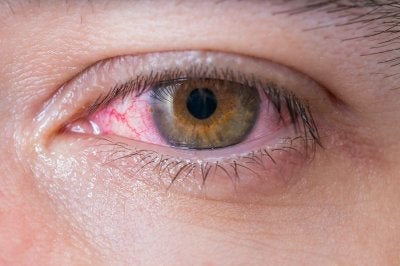
Too much pressure can be bad for your eyes, and it can lead to serious issues that affect your vision. Since vision loss can be permanent, you should practice excellent eye care and talk to your eye doctor in Chicago about how you can protect yourself. You might not notice your symptoms right away, and the disease can continue to progress if you don’t do anything about it. Open-angle glaucoma actually damages your optic nerve, which connects your eyes and brain. Feel free to read ahead if you would like to get the facts about glaucoma.

Symptoms Occur Slowly
Finding out that a given condition doesn’t always have symptoms might seem like a blessing, but sometimes it can do more harm than good. If you don’t notice anything different when you go about your daily life, you probably won’t be in a rush to meet with your eye doctor. When you first develop open-angle glaucoma, there won’t be any symptoms to notice. Everything will feel normal for a period of time, and then your peripheral vision will start to decline. If you don’t visit your eye doctor to create a treatment plan, you may lose your central vision over time as well.
Glaucoma Is Treatable, But Not Curable
Once you have lost some of your vision due to glaucoma, you can’t have it restored. This is why it’s extremely important that you visit your eye doctor for regular checkups. Since you won’t notice any symptoms of the disorder until your vision starts to go, preventative maintenance becomes even more essential. Your eye doctor can prescribe you medication to slow down the progression of the disease by lowering the pressure in your eyes. You can also talk to your eye doctor about surgery or laser trabeculoplasty.
Open-Angle Glaucoma Damages the Optic Nerve
One of the main factors involved in glaucoma is pressure. When fluid won’t properly drain from the eye, you may end up with glaucoma. This retention of fluid ultimately causes the buildup of pressure that damages your optical nerve, which can in turn result in loss of vision.
-
The Patient’s Guide to IOLs
If you’re having trouble with your vision, your eye doctor in Chicago might recommend the use of intraocular lenses , or IOLs. These intraocular implants can help patients deal with certain types of eye diseases, and in doing so they can improve their happiness and comfort. There are a few different kinds of IOLs, and you can discuss the different types with your ophthalmologist to find out which might be right for you. However, they are typically all made of the same material. Read ahead for a quick look at the patient’s guide to IOLs.

When IOLs Are Appropriate
The human eye has many different parts, from the pupils that adjust to let different amounts of light in, to the retinas in the back of the eyes where the images land. When it comes to focusing and visual acuity, you rely primarily on your lenses. Unfortunately, many peoples’ lenses gradually lose strength over time. If you have severe cataracts, then your eye doctor may remove your lens entirely. In this case, the ophthalmologist may replace your original lens with an IOL, which is just an artificial replacement lens. By replacing your cataract lens with a clear new one, you can alleviate issues like blurriness and dulled colors.
Types of IOLs
When you talk to your eye doctor about the possibility of an IOL, you will find that there are quite a few different kinds. A monofocal IOL tends to be the go-to choice after cataract surgery. People typically use these IOLs for distance and wear eye glasses for reading. Toric IOLs are helpful for those with astigmatism, and multifocal IOLs handle both distance and close-up vision. You can also talk to your eye doctor about accommodative IOLs, which can actually change shape after being placed.
What IOLs are Made of
Although there are different kinds of IOLs that you can use after cataract surgery, most of them are made of acrylic or silicone. Additionally, intraocular lenses may help protect your eyes from overexposure to ultraviolet rays. This can prevent additional damage to your eye health in the future.
-
What to Expect from Cataract Surgery
Cataracts are common among older adults. These are areas of clouding on the lens of the eye. If you experience blurry vision, worsening night vision, and halos around light sources, your ophthalmologist will evaluate you for cataracts. It can be alarming to be diagnosed with condition that affects something as precious as your vision, but there is an effective treatment option available: cataract surgery . Discuss what you can expect from the procedure with your cataract surgeon serving Chicago.

Preparing for Cataract Surgery
It may not be necessary to have the procedure right away. Many patients find that their symptoms are barely noticeable. When cataracts grow larger and begin interfering with daily life, your cataract surgeon will help you prepare for the procedure. First, you’ll have a thorough eye exam to measure your eye’s size and shape. You’ll likely be asked not to consume food or liquids for 12 hours before your appointment. It will be necessary to have someone else drive you home from the optical center. You’ll be awake during the procedure, but you won’t be able to feel anything because the cataract surgeon will numb the eye. Some people find it helpful to use a prescribed sedative to help them relax.
Undergoing Cataract Surgery
During this procedure, the ophthalmologist removes the affected lens and implants an artificial replacement, which is known as an intraocular lens (IOL). Your surgeon may perform laser-assisted cataract surgery, which relies on a precise laser to make the incision. The lens is broken up and removed through the incision. Then, the new lens is placed. Stitches usually aren’t required because the incision is tiny. The new lens restores both near and distance vision.
Recovering from Cataract Surgery
Immediately after the procedure, your surgeon will place a protective patch over the treated eye. You’ll rest for about 30 minutes to an hour before a responsible adult can drive you home. Follow your surgeon’s instructions for your recovery, which will include using the eye shield for several hours after the surgery and while sleeping. In addition, your surgeon may ask you to take the following precautions:
- Rest quietly for a few days
- Avoid driving until your eye doctor clears you
- Use eye drops as prescribed
- Avoid rubbing or applying any pressure to the eye
- Go to a follow-up appointment
- Call your eye doctor if side effects develop
It’s normal to experience some discomfort, which should go away within a few days. Expect complete healing in four to eight weeks.
-
Eye Protection for Tennis Players
If you play tennis or plan to learn how, it’s time to schedule an appointment with an ophthalmologist. At an optical center in Chicago, you can learn about the specific risks associated with tennis, including eye injuries that may cause vision loss. Your ophthalmologist can recommend protective eyewear specifically for tennis. He or she will ensure that your eyewear fits you properly for maximum protection.
For more tips on eye care and injury prevention, watch this video. The eye doctor featured here explains that the polycarbonate lenses found in protective eyewear can block projectiles such as tennis balls, even when these objects are traveling at up to 90 miles per hour. She also discusses the importance of ultraviolet (UV) protection to guard against cataracts, lesions, and tumors.
-
Spotlight on the Leading Cause of Vision Loss for Americans Over 60
When it comes to vision loss in seniors, age-related macular degeneration (AMD) is a common problem seen by eye doctors in Chicago . In developed countries, AMD is the leading cause of irreversible vision loss in older adults. If you are nearing age 60 and have concerns about your eye care, then continue reading to learn more about this condition.

The Basics of AMD
At the center of the retina is a small area called the macula, which provides pinpoint vision and enables you to see details clearly. In this way, the macula plays an important role in helping you read, drive, and recognize faces. Macular degeneration refers to the breakdown of the macula, and it’s common for people to develop this condition as a natural part of the aging process. For this reason, age-related macular degeneration is the most common type of macular problem.
The Causes of AMD
Macular degeneration can result from abnormal blood vessel growth beneath the retina. The formation of deposits under the retina, called drusen, are another cause. Studies indicate that genetic changes could be responsible for many cases of macular degeneration, and researchers suspect that the oxidative stress caused by the formation of free radicals in the body may also play a role in the development of AMD.
The Symptoms of AMD
AMD can affect your central vision by causing blurriness, distortion, or dark spots, and this condition rarely impacts the peripheral vision. As an example, someone with advanced AMD might be able to see the outer ring of numbers when looking at a clock, but not the hands in the middle.
The Treatment of AMD
At this time, there is no cure for macular degeneration. However, your eye doctor may recommend several options that can potentially reduce how AMD affects your eyesight and address your symptoms. Supplementation with certain vitamins has been shown to be beneficial, and your eye doctor may also recommend laser therapy, vision aids, or medications as part of your treatment.